Bradycardia, a medical term denoting a heart rate slower than 60 beats per minute in adults, represents a significant concern in cardiovascular health. While some instances of a slow heart rate can be completely normal, particularly in well-trained athletes or during sleep, others signal underlying medical issues that demand immediate attention. Understanding the nuances of bradycardia, from its various forms to the advanced cardiac life support management protocols, is essential for healthcare providers and anyone interested in critical care. The ability to distinguish between a benign slow heart rate and one that indicates hemodynamic compromise is crucial, as timely and appropriate intervention can dramatically alter patient outcomes. This article delves into the complexities of bradycardia, emphasizing the critical role of prompt recognition and adherence to established ACLS guidelines to ensure the best possible care for affected individuals.
Defining Bradycardia and Its Diverse Forms
At its core, bradycardia is defined as a heart rate below the physiological norm for adults. However, this broad definition encompasses a spectrum of conditions, ranging from physiological variations to severe pathological disturbances. Physiologically, bradycardia can be observed in highly conditioned athletes whose hearts are exceptionally efficient, allowing them to maintain adequate cardiac output at lower heart rates. In contrast, pathological bradycardia arises from dysfunction within the heart’s electrical system or due to external factors affecting cardiac rhythm.
The classification of bradycardia helps in pinpointing the origin and severity of the condition. Sinus bradycardia, for instance, originates in the sinoatrial node, the heart’s natural pacemaker, where electrical impulses are generated at a slower-than-usual rate. Junctional bradycardia occurs when the impulse originates from the AV node or the bundle of His, often as a compensatory mechanism when the SA node fails. Heart blocks, on the other hand, involve an interruption in the electrical signals traveling from the atria to the ventricles. These are categorized into first-degree, second-degree (Mobitz I and Mobitz II), and third-degree (complete) heart blocks, each with varying degrees of severity and clinical implications. Idioventricular rhythms, characterized by a very slow rate, originate in the ventricles themselves, often indicating a complete failure of higher pacemaker sites. The array of causes contributing to bradycardia is equally diverse, spanning intrinsic cardiac issues such as sick sinus syndrome and atrioventricular node dysfunction to extrinsic factors like certain medications, electrolyte imbalances, and hypothermia. Medications like beta-blockers, calcium channel blockers, and digoxin are well-known culprits, while conditions such as increased intracranial pressure or even strong vagal stimulation can also lead to a dangerously slow heart rate.
Recognizing the Symptoms and Assessing the Threat of Bradycardia
The presentation of bradycardia can vary significantly, ranging from asymptomatic to life-threatening. The key to effective management lies in differentiating between hemodynamically stable and unstable presentations. Stable bradycardia may present with no noticeable symptoms, allowing for observation and investigation into the underlying cause. Conversely, unstable bradycardia manifests with clear clinical indicators of poor perfusion, signaling that the heart is not pumping enough blood to meet the body’s demands.
Signs and symptoms of hemodynamic compromise are critical alarms that necessitate immediate action. These include hypotension, where blood pressure drops to dangerously low levels, altered mental status indicating reduced blood flow to the brain, and overt signs of shock, such as cool, clammy skin and rapid breathing. Patients might also complain of chest pain, a sign of myocardial ischemia due to inadequate oxygen supply to the heart muscle, or symptoms of acute heart failure, such as shortness of breath and fluid accumulation. A thorough risk assessment is paramount, considering patient factors that increase susceptibility, such as pre-existing cardiac conditions and age, as these can influence the severity and prognosis of bradycardia. The immediate consequences of untreated unstable bradycardia can be dire, potentially leading to cardiac arrest, underscoring the urgent need for intervention.
The ACLS Bradycardia Algorithm: A Systematic Approach to Treatment
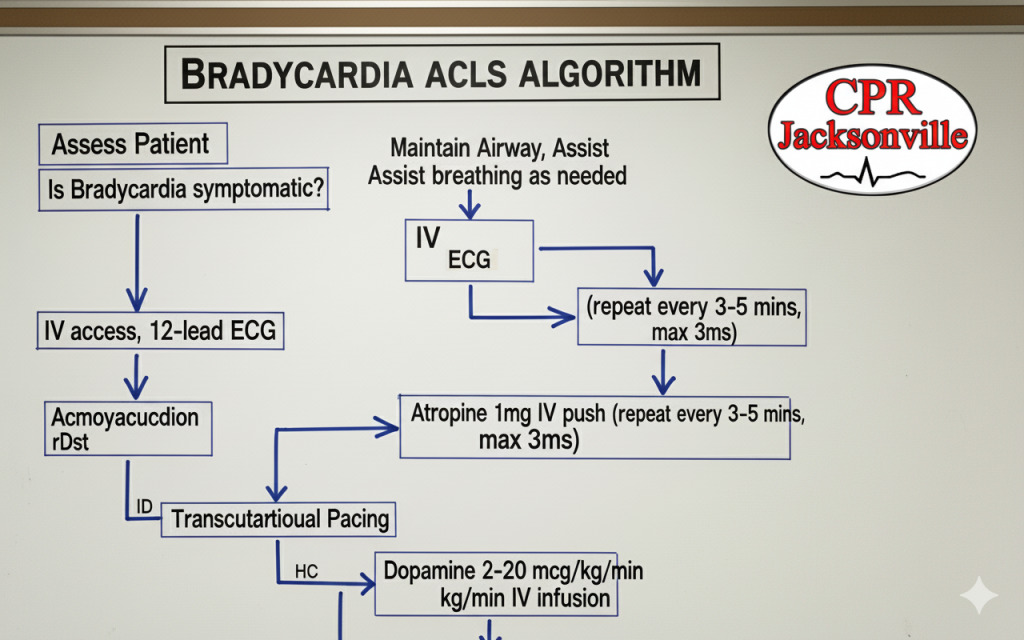
The Advanced Cardiac Life Support bradycardia algorithm provides a structured, systematic approach to the assessment and treatment of patients experiencing a slow heart rate. This decision-making flowchart guides healthcare providers through a series of steps, ensuring that critical interventions are administered promptly and effectively. The process begins with a primary assessment, focusing on the patient’s airway, breathing, and circulation, followed by a pulse check and rhythm identification. Concurrently, blood pressure and oxygen saturation are measured to gauge the patient’s overall hemodynamic status. This initial phase rapidly establishes the severity of the situation and whether the patient is stable or unstable.
Following the primary assessment, a secondary assessment is performed, including a 12-lead electrocardiogram to precisely identify the type of bradycardia and signs of hemodynamic compromise. Simultaneously, healthcare providers investigate and address any potentially reversible causes of the bradycardia, such as electrolyte imbalances or medication effects. Based on the assessment, treatment interventions are initiated. Pharmacological interventions are often the first line of defense. Atropine, a cholinergic antagonist, stands out as the primary medication used to treat symptomatic bradycardia. It works by blocking vagal stimulation, thereby increasing the firing rate of the SA node and improving AV conduction, often leading to a rapid improvement in heart rate. The recommended dosage for atropine is 1 mg IV/IO, which can be repeated every three to five minutes up to a maximum total dose of 3 mg.
When atropine proves ineffective or is contraindicated, advanced interventions become necessary. Transcutaneous pacing (TCP) is a vital intervention for hemodynamically unstable bradycardia that does not respond to atropine. TCP involves delivering electrical impulses through the chest wall to stimulate myocardial contraction, effectively setting a temporary heart rate. Proper application technique, including pad placement and setting appropriate rate and output, is critical for successful capture. In addition to pacing, chronotropic medications such as epinephrine infusion (2-10 mcg/min) and dopamine infusion (5-20 mcg/kg/min) can be used to increase heart rate and improve cardiac output. Isoproterenol may also be considered in specific circumstances, though its use requires extreme caution. Ultimately, definitive treatment for persistent or severe bradycardia may involve transvenous pacing or the consideration of a permanent pacemaker, especially in cases of chronic or recurrent symptomatic bradycardia.
The First Intervention for Bradycardia and Beyond
In managing bradycardia, the immediate priority revolves around ensuring the patient’s basic physiological needs are met while simultaneously addressing the slow heart rate. The initial response involves a primary survey and stabilization efforts. This means ensuring adequate oxygenation and ventilation by providing supplemental oxygen as needed, establishing intravenous or intraosseous access for medication administration, and initiating continuous cardiac monitoring to observe the heart rhythm and assess the effectiveness of interventions.
Atropine is often the first-line pharmacological agent due to its rapid onset of action and its ability to effectively block the parasympathetic nervous system’s influence on the heart, which can slow the heart rate. It is particularly effective in treating bradycardia caused by increased vagal tone. However, it is important to recognize when atropine may not be effective, such as in cases of complete heart block, in patients with transplanted hearts where vagal innervation is absent, or in high-degree AV blocks occurring below the AV node. In such scenarios, or when atropine fails to achieve the desired response, clinicians must be prepared to quickly transition to transcutaneous pacing.
The step-by-step management of bradycardia in ACLS unfolds in distinct phases. The initial response, typically within the first zero to two minutes, involves assessing responsiveness and pulse, applying monitors and oxygen, obtaining IV/IO access, and identifying the cardiac rhythm. The intervention phase, spanning two to five minutes, focuses on assessing for hemodynamic compromise, administering atropine if indicated, and preparing for transcutaneous pacing. In cases where pacing is necessary, patient preparation, including sedation to manage discomfort, proper pad placement, and careful adjustment of rate and output settings, is crucial. Ongoing management, extending beyond five minutes, includes continuous monitoring of the patient’s response to interventions, preparing for advanced interventions like transvenous pacing if needed, considering expert consultation, and planning for definitive long-term care.
Special considerations and contraindications are also important. For atropine, while generally safe, relative contraindications include angle-closure glaucoma and obstructive uropathy. For transcutaneous pacing, ensuring patient comfort and monitoring for effective electrical capture are paramount. Pediatric patients present unique challenges, requiring different heart rate thresholds, weight-based dosing for medications, and alternative approaches tailored to their physiological differences. Case studies, ranging from hemodynamically stable bradycardia where observation might be appropriate to unstable bradycardia requiring rapid, multi-modal intervention, and cases not responding to initial treatment, provide valuable learning opportunities to refine clinical decision-making.
The Critical Importance of Training and Certification
The effective management of bradycardia, especially in emergent situations, hinges significantly on the proficiency and preparedness of healthcare providers. This underscores why proper ACLS training and certification are not merely bureaucratic requirements but fundamental pillars of patient safety and optimal outcomes. The ability to quickly recognize the signs of critical bradycardia and implement the correct interventions within the tight window of opportunity can literally mean the difference between life and death. Hands-on practice, particularly through simulation scenarios, is invaluable in developing the muscle memory and critical thinking skills required to navigate high-pressure situations. A team-based approach, fostered through regular training, ensures seamless coordination and communication among healthcare professionals during a cardiac emergency.
Training centers, such as CPR Jacksonville FL, play a pivotal role in equipping healthcare providers with these life-saving skills. Offering American Heart Association-certified courses, these centers provide a stress-free, hands-on learning environment conducive to mastering complex algorithms and procedures. From Basic Life Support (BLS) for Healthcare Providers to Advanced Cardiac Life Support (ACLS) and Pediatric Advanced Life Support (PALS), and even general CPR and First Aid, these programs ensure that medical professionals are well-versed in the latest guidelines and techniques. Such comprehensive training not only ensures initial certification but also provides